
Seriously
Mental Health Care for Prison Inmates
11/15/2013 23:46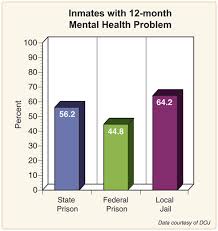 Abstract
Abstract
There are 8 countries as of 2012 according to (Park, 2012) that offer free or healthcare to the citizens. For example, Brazil - population 199,321, Moldova – population 3,656,843, Kuwait – population 3,328,136 offers free health care coverage. Whereas countries like China, Chile and Rwanda may not offer free coverage for every citizen, they are working on some feasible solutions to providing health coverage. The United States population as of November 13, 2013 was 317, 061,796 as per the United States Census Bureau (www.census.gov). Within the population of the U.S., there is a segment of citizens that were incarcerated as of 2012, that number was 6,977,700 (Glaze, 2012). According to (“Health insurance costs,” 2013) the yearly average cost of health care per person was $5,615 per year. If the U.S. at $5,615 per person covered everyone, the U.S. would spend approximately $1.780, 301,984,540 per year less $39,179,785,500 for the inmate population. The rate of recidivism would dramatically reduce if mental and physical health services were allowed to be accessed in prison (see Figure 1). At a whopping rate of $7.15 per day according to (Kinsella 2004) under the proposed 2014 Healthcare Reform offering care to inmates should speak for itself.
Mental Health Care for Prison Inmates is it Cost Effective Under the Patient the Patient Protection and Affordable Care Act (PPACA).
PPACA is a law that establishes how every citizen will access health care in the year 2014. It is designed to expand coverage, improve the delivery of care and monitor health care costs. According to Kaiser’s report ("Summary of the,”) the uninsured are low-income families, people of color and non-Hispanic Whites. The report does not identify prison inmates in the population of uninsured (those without insurance) or in the underinsured (those without adequate coverage) population. The Affordable Care Act legislation states in section 1312 states, “ Within section 1312, the legislation states, “all qualified individuals may purchase qualified health plans” and “[a]n individual shall not be treated as a qualified individual if, at the time of enrollment, the individual is incarcerated, other than incarceration pending the disposition of charges [emphasis added].” (Grossman, 2010). Why are jails and prisons not mandated to provide coverage for inmates? Furthermore the law defines a qualified individuals a person who lives in a State that offers the Exchange and is looking for coverage through the Exchange but is not incarcerated, (Grossman 2010) however, if the person has not been sentenced they are considered “qualified”. Unless our jails and prisons have become a warehouse for the mentally ill, the PPACA should reconsider the inclusion of the prison inmates.
The Role of the Prison System
With the corruption and abuse in the prisons in the British jails reform was demanded. Ten years later the United States began to look at prison reform. The corruption described in the book titled Report on the Prisons and Reformatories of the United States and Canada by Enoch Wines and Theodore Dwight, identified corruption and prisoner abuse. The first prisons according to (Meskell, 1999) were a combination of colonial criminal law and religion. Criminal punishment was immediate and regulated by the community. There were public humiliations public penances. The punishment was designed to deter criminals from acting out. Has the present day system of incarceration-deterred criminals from repeating the behavior that led to the initial arrest and conviction, I think not.
Presently the atmosphere in prisons relative to those that mental health issues are such that they are abused by the other inmates, they are out casted with by being forced to wear different colored jail uniforms than those of the regular population. They are sometimes referred to, as “ding-a-lings” and the verbal abuse are commonplace in the facilities. One important fact is that the mentally ill may not know how to navigate the institution or understand the rules and regulations. The tragic stench of suicide occurs all too often, data from a 1977 report noted that half of all inmates that committed suicide had been previously hospitalized for a mental disorder (Torrey, 1995). (Teed & Scileppi, 2007) Explains the process of deinstitutionalization with first understanding the process of “institutionalization”. Physicians were unable to accurately identify or diagnose the illness, which led to a host of inhumane treatment for the mentally ill population to include locking them away in a facility without proper care and/or treatment. Much like the prison facilities today, not much or no care is provided for the mentally ill. The work conducted to change the trajectory of institutionalization has been re-routed to the prison system. The United States jails more individuals than any other nation with costs exceeding $9 billion in California alone based on a report from (Gascón, 2013).
The issue with providing mental health costs is will each state implement the mandate for providing Medicaid to the uninsured by the year 2014. The Federal Government provides a funding source for each state that elects to expand Medicaid to the uninsured, paroled inmates, those on probation and those presently incarcerated. However if the state declines the expansion the state will still receive the funding however, those incarcerated, released on parole or probation will not have coverage. For those needing substance abuse treatment from a facility will not have the opportunity to be admitted, if relapse occurs the behaviors associated with addicts will reform and possible incarceration will be repeated. For those with bi-polar or anxiety issues may not get to see a therapies or psychiatrist and medication will not be offered and the behavior which led to incarceration could present itself again.
(Braude, & Miller) provides a 10 step program to improved the outcomes of inmates:
1. Standardized screens for behavioral health needs – universal screenings and/or assessments;
2. Verify Medicaid eligibility which was not previously part of the prison system;
3. Preserve existing benefits – This would aid in the inmate during the release process to ensure a “continuity of care” if you will making sure they can get into a facility immediately upon release vs. waiting for coverage to be approved by the state;
4. Assistance in applying for benefits – Applications should be completed prior to a prisoners release to ensure they are covered upon release;
5. Coordination of benefits - identify if the prisoner has any other source of coverage prior to release;
6. Information sharing – This would be a great process to ensure that the agencies can share information based on the inmates consent prior to release;
7. Benefit Enrollment – Complete all paperwork prior to release to ensure enrollment at the time of release;
8. Facilitate enrollment – Inmates can be paroled directly into a facility this would reduce re-entry if the inmate has an addiction issue.
9. Build community partnerships – a collaborative system of care for parolees could ensure that the inmate is not faced with a barrage of “to-dos” that they may be unfamiliar with relevant to health care.
10. Med Management – Inmates are supplied with a limited supply of medication according to the article – this may require additional research.
Finally what is the impact to the provider, again (Braude, & Miller) provides 10 steps to identifying the impact of PPACA in the behavioral health care field.
1. Coverage will expand for every state;
2. Medicaid recipients will increase;
3. Community bases work-around will surface to cover the uninsured;
4. Behavioral health benefits will be monitored because of the proposed influx of recipients the resources could be extinguished sooner rather than later;
5. The whole person will have to be implemented i.e. incorporating family support into the treatment process as well as addressing the physical issues of the individual.
6. Partnerships in this sector will have to be drawn and/or nurtured to handle the number of recipients.
7. Recruitment of professional to handle the population;
8. Organized information technology
9. State level Mental Health Parity – providers must heed to the syllabus.
10. Fiduciary responsibilities and needs must be accurately determined to ensure process flow of every organization.
What is the solution to providing care for the mentally ill population in the prison system depends on the voice of the loved ones and the concern of mental health providers.
References
Braude, L., & Miller, N. (n.d.). Using health reform to enhance health outcomes for former inmates. Retrieved from https://www.rsat-tta.com/Files/PPACA_Improving-the-Return
Bureau of Justice (n.d.). Bureau of Justice Statistics (BJS). Retrieved November 13, 2013, from https://www.bjs.gov/index.cfm?ty=tp&tid=11
Gray, Katti (2012, August). The prison health care dilemma. Retrieved from https://www.thecrimereport.org/news/inside-criminal-justice/2012-08-the-prison-health-care-dilemma
United States Census Bureau (n.d) U.S. and World Population Clock. Retrieved November 13, 2013 from https://www.census.gov/popclock/
Glaze, L. E. (2012, November 29). Correction populations in the United States 2011. Retrieved from https://www.bjs.gov/index.cfm?ty=pbdetail&iid=4537
Grossman, E. G. U.S. House of Representatives, (2010).Compilation of patient protection and affordable care act. Washington, DC: Office of the Legislative Counsel.
Gascón, G. (2013, March 19). Time for sentencing reform. Retrieved from https://www.thecrimereport.org/viewpoints/2013-03-time-for-sentencing-reform
Health insurance cost statistics. (2013, July 7). Retrieved from https://www.statisticbrain.com/health-insurance-cost-statistics/
Kinsella, C. The State Council of State Governments, (2004). Corrections health care cost. Retrieved from website: https://www.prisonpolicy.org/scans/csg/Corrections Health Care Costs 1-21-04.pdf
Summary of the affordable care act. (n.d.). Retrieved November 13, 2013 from website www.kff.org
Meskell, M. W. (1999). An American resolution: the history of prisons in the united states from 1777 to 1877.JSTOR, 51(4), 839-865. Retrieved from https://jthomasniu.org
Park, M. (2012, June 29). Where in the world can you get universal health care? Retrieved from https://www.cnn.com/2012/06/28/health/countries-health-care
Torrey, E. F. (1995). Jails and prisons - America's new mental hospital. American Journal of Public Health, 85(12), 1611-1613. Retrieved from https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.85.12.1611
Teed, E. L., & Scileppi, J. A. (2007). The community mental health system. (p. 28). Boston, MA: Pearson Education, Inc.
Tags:
—————
